Testosterone Replacement Therapy.
Our TRT Program Pricing Is Simply Unbeatable – GUARANTEED !
![]()
Show us a lower price and we’ll beat it.
Telehealth Physicians | Licensed in All 50 States.
“We Are The Best Priced TRT Clinic in America, Guaranteed.”
Cost of Treatment
TRT – Testosterone Replacement Therapy
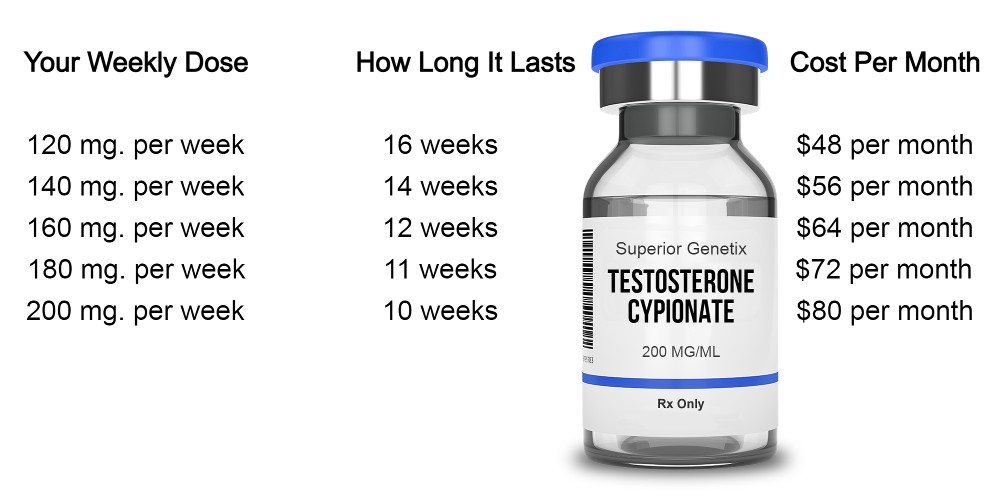
$200 / Provides You 10 to 16 Weeks of Treatment & Includes:
- Testosterone Cypionate (200mg./ml.) 10ml. vial
- Aromatase Inhibitor blend (if medically necessary).
- Injection Kit. Syringes and Needles To Your Specifications and Alcohol Pads
- Unlimited Email Support
- Phone Consultations With a Specialist (Appointment Required)
What Is Not Included
- Fertility/atrophy treatments such as Gonadorelin, HCG, or Enclomiphene.
- Blood work that you request, that is not required for your treatment.
- Additional Physician Consultations That You Request
- Shipping & Handling is $20 Per Order
*The pharmacies may charge different shipping rates for the following states: ALABAMA, ARKANSAS, CALIFORNIA, KANSAS, MICHIGAN, , MINNESOTA.
Cost To Add On
- Fertility/Atrophy Treatment With Gonadorelin: $120 for a 60 day supply
- Fertlitity/Atrophy Treatment With Enclomiphene (12.5mg): $125 per 60 day supply
- Blood Work On Demand : Click Here For Prices
- Want To Make An Additional Appointment With One of Our Physicians ? The Cost Is $150
How To Get Started
- Complete The New Patient Intake Form
- Pay The Intake Fee
- Get Your Labs (if applicable)
- Do Your Pre-Appointment Consultation With One of Our Specialists. This is where we answer all of your questions, and provide you with instructions on how to get the most out of your treatment.
- Do Your Brief Appointment With The Prescribing Physician
- Pay For The Treatments You Select
![]()
Have Questions ? Click Here To Contact Us
Ready To Get Started ?
To begin the process, click the button below and complete the New Patient Forms.
After you have completed the intake forms, you will receive a welcome email from our client intake manager who will answer any questions you might have.


